Electromyography ALS, a diagnostic procedure involving the examination of muscle and nerve functioning, has played a vital role in the detection of Amyotrophic Lateral Sclerosis (ALS), a progressive neurodegenerative disorder. This article delves deep into the valuable insights that can be gleaned from needle EMG findings and the fascinating patterns of denervation witnessed in patients suffering from this disease.
Understanding Electromyography ALS
Electromyography (EMG) is a diagnostic procedure utilized to evaluate the health condition of muscles and the nerve cells controlling them (the motor neurons). ALS, one of the illnesses detected by EMG, attacks the motor neurons in the brain and spinal cord, leading to muscle weakness and atrophy.
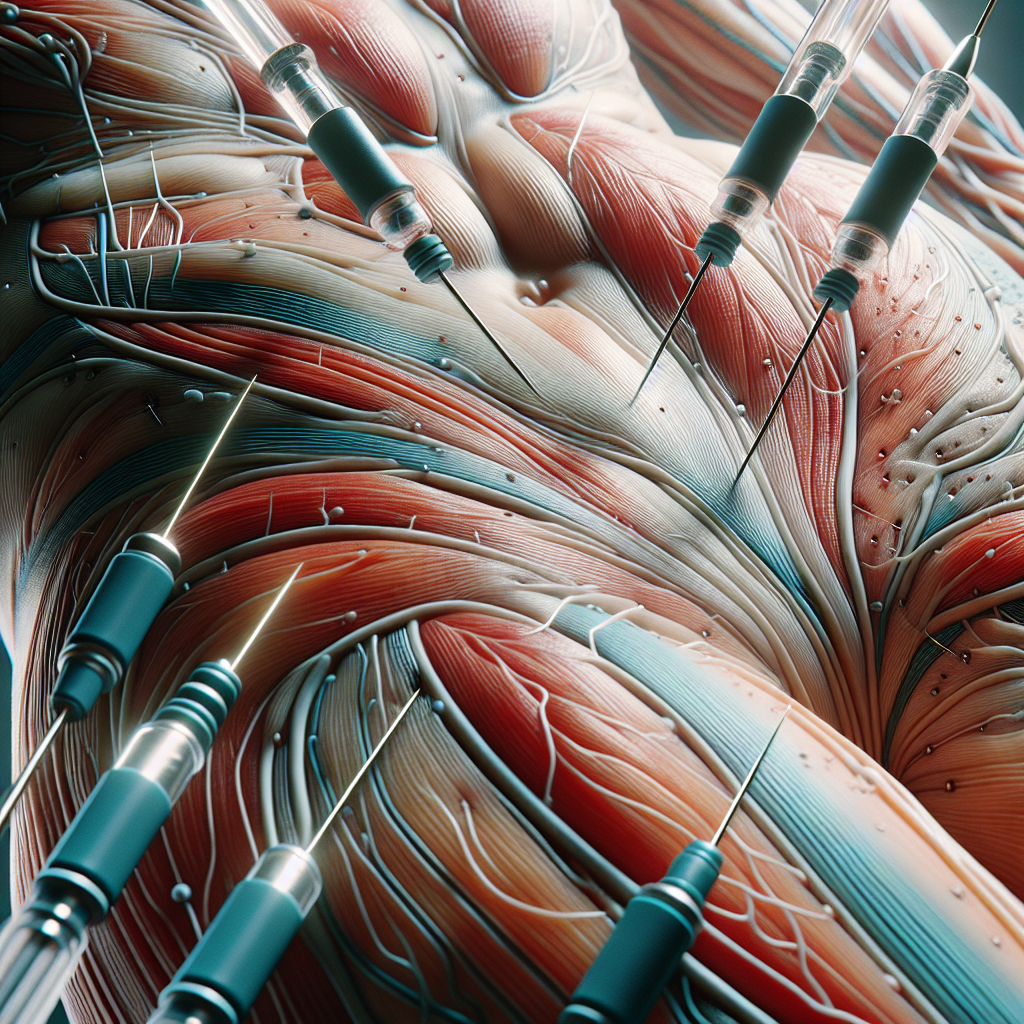
Notably, needle EMG enables researchers and healthcare practitioners to identify symptoms typically associated with ALS. The procedure involves inserting a needle electrode into a muscle to assess its electric activity during contractions and when at rest. This data can help spot abnormalities potentially indicating ALS.
Decoding Needle EMG Findings in ALS
Needle EMG findings can reveal fascinating insights into the progression and severity of ALS. Spontaneous activity, such as fibrillations and positive sharp waves, usually indicates a potential onset of ALS.
Furthermore, fasciculations (muscle twitching) and high amplitude motor unit potentials can also signal impending ALS. Neurologists, in particular, use these signals to track the disease, gauge its severity, and implement suitable treatment methodologies.
ALS and Denervation Patterns: A Closer Look
Electromyography ALS can help observe denervation, a condition linked to damage to the nervous system where moves lose their nerve supply. ALS typically exhibits both active and chronic denervation. Identifying such denervation patterns becomes significantly crucial in diagnosing ALS.
In ALS, muscle weakness usually begins in one area and progressively spreads to other regions of the body. This denervation pattern, known as “dying back” or “length-dependent” denervation, commonly starts in distal extremities (e.g., hands and feet), gradually moving towards the body’s central parts.
Compellingly, recent research has unearthed a subtype of ALS, characterized by a “non-length dependent” denervation pattern. In these instances, the denervation process starts in proximal regions (such as the trunk or shoulder region) and spreads to the distal areas.
Conclusion
Electromyography ALS, with its illuminating observations from needle EMG findings and denervation patterns, can be instrumental in identifying ALS and managing its devastating effects. Early detection can aid in improving a patient’s quality of life and deploying potential treatments. It underscores the importance of periodic neurological examinations and EMG tests, especially for individuals at risk of developing such conditions.
However, more research remains crucial to explore novel diagnostic strategies and ensure a more accurate and early detection of ALS.
If you or your loved one is coping with ALS symptoms and believe exposure to Real Water may have contributed, be proactive. Visit the lasvegasalsrealwater.com’s contact page to get the necessary assistance. Explore more related content on understanding ALS and its various aspects on the website’s blog page. If immediate assistance is necessary, do not hesitate to call 702-385-6000.
References
– Electromyogram (EMG) Test & Results Interpretation
– Amyotrophic Lateral Sclerosis (ALS) – Symptoms and Causes
– Non-length dependent and length-dependent ALS, two distinct clinical entities